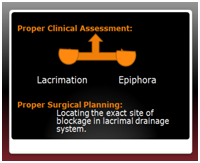
 Clinical Assessment: In a patient presenting with a watery eye, it is very important to distinguish whether the watering is due to excessive tear production (lacrimation) or due to poor drainage from the lacrimal system (epiphora). Normally, there is a state of balance between tear production and drainage by the lacrimal system; some tears are lost by evaporation and the remaining fall within the capacity of the lacrimal system hence not everybody suffers from this problem.
Clinical Assessment: In a patient presenting with a watery eye, it is very important to distinguish whether the watering is due to excessive tear production (lacrimation) or due to poor drainage from the lacrimal system (epiphora). Normally, there is a state of balance between tear production and drainage by the lacrimal system; some tears are lost by evaporation and the remaining fall within the capacity of the lacrimal system hence not everybody suffers from this problem.
History
A careful history will elucidate the extent of problem and its cause. Hence it is important to ask certain pertinent questions:
1) Duration of the watery eye, whether unilateral or bilateral.
2) Whether accompanied by pain, irritation, itching, burning or stinging in the eye.
3) History of accompanying mucoid or purulent discharge in the eye.
4) Previous treatment: eyedrops, S/P, surgery.
5) History of previous trauma to the medial side of orbit or nose.
6) History of nasal obstruction, chronic sinusitis.
7) General health: patient may need surgery under a local or general anaesthetic; the local anaesthetic contains adrenaline for haemostasis. They need to stop anticoagulants, blood thinners 5 days prior to surgery. Diabetes and hypertension should be under control prior to surgery.
Examination
Aim of examination is to decide whether the problem is lacrimation, epiphora or a combination of the two and to decide regarding management.A detailed examination is mendatory and should include:
1) Lids: blepharitis, meibomitis, conjunctivitis, trachoma, fistula, lid laxity with scleral show and lateral lower lid droop (pooling of tears laterally), facial palsy (lacrimal pump failure).
2) Lacrimal punctae: patency, positioning.
3) Lacrimal sac area: look for swelling, redness, fistula, surgical scar mark.
4) Press on the lacrimal sac and note regurgitation of mucus, pus, mucopus.
5) Nasal examination: deviated nasal septum, polyps.
6) Fluorescein Dye disappearance Test: a drop of 2% fluorescein is instilled into the conjunctival sac. A cotton swab is placed in the inferior meatus of nose. After 2 min. if the dye can be seen on the swab, the test is positive and lacimal system is assumed to be patent. If no dye is recovered, the system is syringed. If the dye appears this time, this is a positive secondary test and indicates partial obstruction in the cannaliculi.
7) Syringing &Probing: this is a very important test and should determine the exact site of blockage in the lacrimal drainage system. It can be done in the clinic with the patient comfortably lying down. Local anaesthetic drops are instilled into the conjunctival sac. Punctae are dilated first with a punctum dilator. Then a No. 00 Bowmann’s probe is gently introduced into the lower punctum. The lower lid is drawn laterally to avoid kincking of the inferior and the common cannaliculus as the probe is advanced forwards into the lacrimal system. If a soft stop is felt, the probe is not advanced any further forcibly to avoid making a false passage. Its lateral end is held with a forceps and the length it traversed into the lacrimal cannaliculus is measured with a ruler. This measurement will identify the exact site of blockage.
Next, the system is syringed by a lacrimal cannula introduced into the inferior cannaliculus and irrigated with saline while the lid is gently drawn laterally to avoid kincking of the cannaliculus. If the saline regurgitates from the upper punctum and some flows into the nasopharynx, this indicates a partial block in the inferior or common cannaliculus.
Hence, probing determines the exact site of block.If there is free flow of saline into the nasopharynx, Syringing shows that the whole system is patent; if some fluid regurgitates and some flows into the nasopharynx, then there is a partial blockage in the system. A combination of both decides for the exact surgical procedure.

Punctal dilatation.Probe introduced into the punctum, introduced medially while lid is drawn laterally. Probe is held with forceps just lateral to punctum before being removed, then the length measured with a ruler.
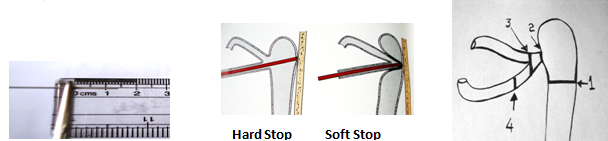
S/P
1: NLD block (hard stop) DCR
2: Common cannalicular block (Medial soft stop) DCR + Intubation
3: Common cannalicular block (lateral soft stop) >7mm CDCR
4: Cannalicular block, soft stop <7mm L.J.Tube
Locating the exact site of blockage in the lacrimal drainage system PRE-OPERATIVELY is mandatory for a successful outcome.
Note: for further reading regarding Lacrimal Surgery, consult my book, “An Insight into Oculoplastics” available at my Bookshop.